Arthritis is a common condition that affects millions of people, and it can occur in various joints in the body. When it comes to the hand, one of the areas that can be affected is the base of the thumb. Imagine feeling pain from something as simple as turning a key or snapping your fingers. For many, this constant reminder is unbearable. This condition, known as thumb arthritis, can lead to pain, swelling, and reduced hand function. Let’s explore what thumb arthritis is, its symptoms, causes, risk factors, diagnosis, and available treatment options. If you’re suffering from this condition, we hope we can help.
What is Thumb Arthritis?
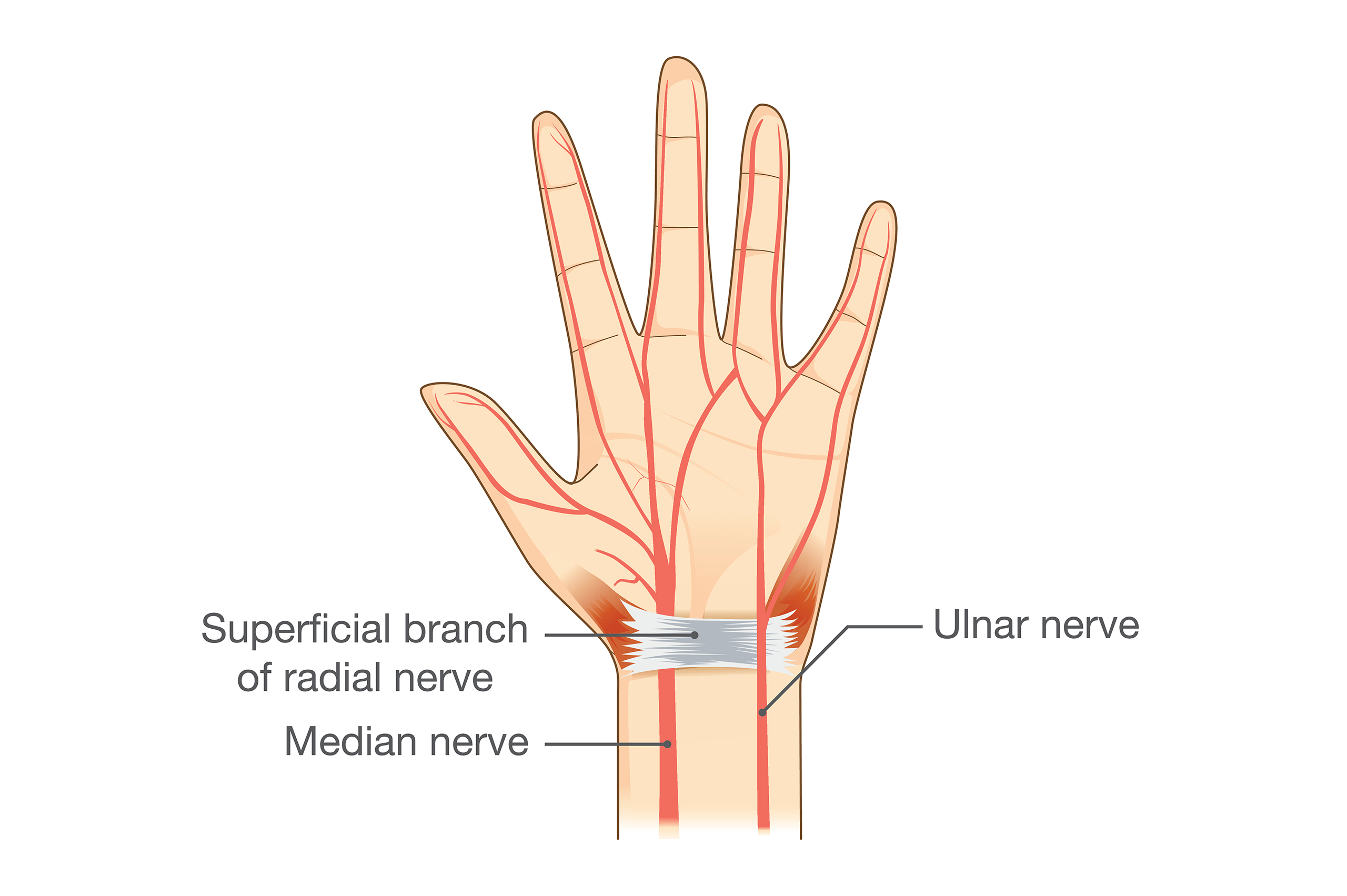
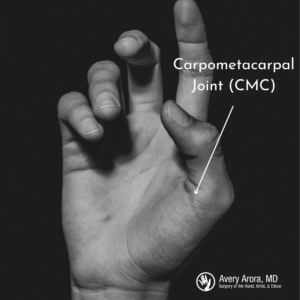
Thumb arthritis primarily affects the joint at the base of the thumb, making it the second most common site of arthritis in the hand. It’s typically a form of osteoarthritis (OA), which results from the gradual wear and tear on the joint. In a healthy joint, cartilage acts as a cushion between the bones. However, in people with thumb arthritis, this cartilage wears away, leading to bone-on-bone friction, inflammation, and pain.
Symptoms of Thumb Arthritis
The most common and early symptom of thumb arthritis is pain at the base of the thumb, especially during activities that involve gripping, pinching, or applying force with the thumb. Other symptoms may include swelling, aching, discomfort, tenderness, limited range of motion, an enlarged appearance at the base of the thumb, and reduced thumb strength. These symptoms tend to worsen over time, especially without treatment.
Thumb Arthritis Causes and Risk Factors
Thumb arthritis is primarily caused by the gradual breakdown of cartilage over time, which is often associated with aging. Injuries, such as thumb fractures and dislocations, can also lead to this condition. In rare cases, joint infections may be responsible for thumb arthritis.
Several risk factors can increase the likelihood of developing thumb arthritis, including age, gender (with females being more prone), weight, genetics, joint laxity, hormonal changes (such as menopause), previous joint injuries, and certain occupational factors. You can read more about what causes thumb arthritis on our website’s dedicated thumb arthritis page.
Diagnosis of Thumb Arthritis
To diagnose thumb arthritis, a healthcare provider such as top doctor Avery Arora, MD will conduct a physical examination, assess pain levels, and inquire about prior thumb injuries and the patient’s medical history. X-rays are often used to visualize joint space, cartilage loss, and the presence of bone spurs, which are indicative of arthritis.
Thumb Arthritis Treatment Options
While there is no cure for arthritis, there are various treatment options available to manage thumb arthritis:
Non-surgical Treatments:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation.
- Counterirritants that distract from pain.
- Corticosteroids to reduce inflammation.
- Analgesics for pain relief.
- Physical therapy and exercises to strengthen thumb muscles.
- Wrist supports and braces.
- Activity modification to reduce thumb stress.
Surgical Measures:
- Total joint replacement.
- Fusion surgery to eliminate pain by fusing the bones.
- Ligament reconstruction to stabilize the joint.
- Ligament reconstruction and tendon interposition (LRTI) to prevent bone friction.
In severe cases, surgery may be required. Recovery from surgery may take several weeks to months and may involve working with a physical therapist.
Finding Relief from the Pains of Thumb Arthritis
Thumb arthritis is a common condition that can cause discomfort and limitations in hand function. While it cannot be cured, there are various treatments available to manage symptoms and improve quality of life. Early diagnosis and appropriate management are essential for individuals dealing with thumb arthritis.
If you suspect you have thumb arthritis or are experiencing thumb pain, there are many reputable hand doctor options from the Ascension or Beaumont healthcare systems or you can seek assistance from a qualified medical professional at a private practice. Arora Hand Surgery, led by Dr. Avery Arora, a specialist in upper extremity problems and a top Michigan hand doctor, has helped countless individuals alleviate their thumb arthritis symptoms. You can contact the practice, with four locations in West Bloomfield, Warren, Macomb, and Howell, at (888) 392-4263 or schedule your consultation







 You will need a large amount of dental floss to do this. Start by threading it under the ring so you have a “pull” handle of floss facing the wrist. The rest of the floss will be facing your fingers.
You will need a large amount of dental floss to do this. Start by threading it under the ring so you have a “pull” handle of floss facing the wrist. The rest of the floss will be facing your fingers.